History of the kidney disease treatment

The concept of a dialyser was first conceived by Scottish chemist Thomas Graham. A machine successfully developed for patients was eventually created nearly 90 years later by Dr Willem Kolff. The first patient in the world to be treated by repeated haemodialysis was Clyde Shields, whose first dialysis was in Seattle, USA, on March 9th 1960. Developments in access to the blood system and a new forms of dialysis using peritoneum followed. The result, millions of lives saved and transformed. Transplantation further revolutionised the life expectancy and quality of life for patients as immunosuppressants were developed and improved alongside the use of living donors.
|
Scottish chemist Thomas Graham, known by some as the 'father of dialysis', first described dialysis in 1854. He used osmosis to separate dissolved substances and remove water through semi-permeable membranes, although he did not apply the method to medicine |
Thomas Graham's Dialyser.
|
The first human dialysis machine
Dr. Willem Kolff (1911-2009) is considered by most to be the father of dialysis. This young Dutch physician constructed the first dialyzer (artificial kidney) in 1943.
|
|
Kolff’s work to create of an artificial kidney began in the late 1930s when he was working in a small ward at the University of Groningen Hospital in the Netherlands. There, Kolff watched helplessly as a young man died slowly of kidney failure. Kolff decided to find a way to make a machine that would do the work of the kidneys. At about the same time that Kolff began his research, World War II erupted. Once the Nazis overtook the Netherlands, Kolff was sent to work in a remote Dutch hospital. Although materials were scarce, Kolff improvised, using sausage skins, orange juice cans, a washing machine and other common items to make a device that could clear the blood of toxins. |
|
In 1943, Kolff’s invention, although crude, was completed. During the course of the next two years, he treated 16 patients with acute kidney failure but had little success. All that changed in 1945, when a 67-year-old woman in uremic coma regained consciousness after 11 hours of haemodialysis with Kolff’s dialyzer. She lived seven more years before dying of another ailment. Kolff’s machine is considered the first modern drum dialyzer, and it remained the standard for the next decade. After World War II ended, Kolff donated the five artificial kidneys he’d made to hospitals around the world, including Mt. Sinai Hospital in New York. He later moved to this hospital to continue his research. |
|
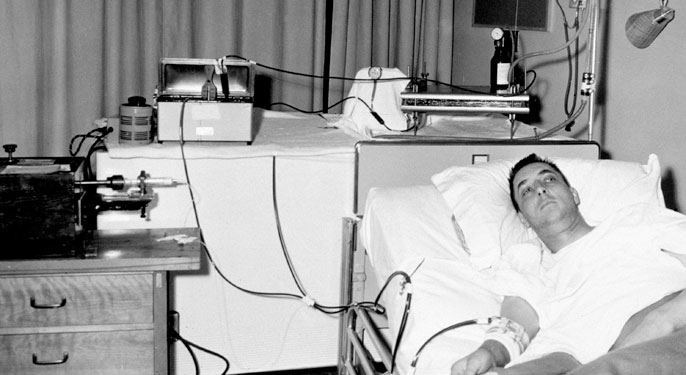
The first patient in the world to be treated by repeated haemodialysis was Clyde Shields, whose first dialysis was in Seattle, USA, on March 9th 1960. For several decades some patients with Acute renal failure had been lucky enough to be treated by haemodialysis. They were treated until their kidneys started working again. |
|
Access to large veins, however, was by means of metal cannulae, and the 'lines' were opaque rubber tubing. The cannulae would have to be inserted at each dialysis. Infection of the access sites was a common problem. Typically, the patients treated were oligo-anuric (urine output less than 100ml per day); treatment continued until urine flow returned. If the patient remained oligo-anuric, the process was usually discontinued after 6 weeks.
This meant that patients with chronic kidney disease (CKD) were left untreated to die.
There were two technical advances that led to the possibility of long-term haemodialysis treatment - the introduction of Teflon and a siliconised plastic called 'Silastic'. The patient would need to have an arterio-venous shunt fitted - usually in the forearm or lower leg. A 'Scribner' shunt consisted of a length of Silastic tube at either end of which was a piece of Teflon tube that would be tied into the vessel [one for the artery, one for the vein]. The important aspect was that blood from the artery flowed through the Silastic portion to the vein. A bandage covered the sites of insertion, and a portion of the Silastic tube left visible. The patient could by feeling the temperature of the tubing [should be blood temp, not cold] check that blood was flowing from artery to vein, and not stationary [i.e. clotted]. The Silastic portion had a break in the middle [connected by Teflon tube] so that the two halves could be separated for use at dialysis.
Dialysis in the UK
The first maitenance haemodialysis unit in the UK was opened by Stanley Shaldon at the Royal Free Hospital in 1961. This was followed by David Kerr at Newcastle in 1963 and Hugh de Wardener at the Charing Cross Hospital in April 1964. Stanley Shaldon also launched the first home HD programme in 1964
|
|
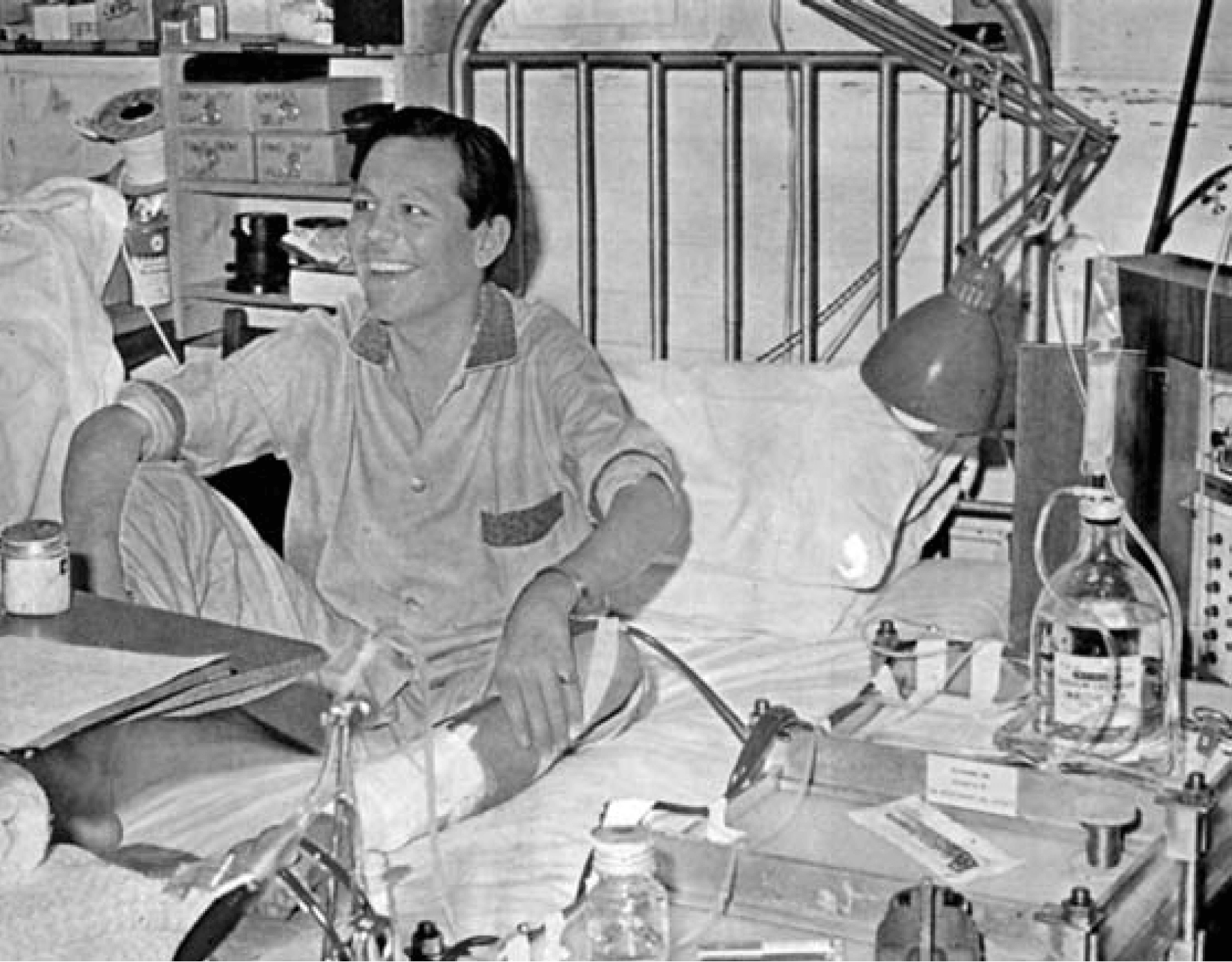
Robin Eady (later Emeritus Professor of Dermatology at King's College London) receiving haemodialysis in the ‘side room’ of the Royal Free Hospital renal unit in 1966. On 26 February 2008, a Witness Seminar on the development of dialysis in the UK (1950-80), was held at the Wellcome Trust Centre for the History of Medicine at UCL, London (Crowther, 2009). The transcript of this meeting is well worth reading for personal accounts of this pioneering time for renal services in the NHS. |
In the last four decades, the major developments have been related to improvements in membrane biocompatibility and dialyser design, volumetric control, sophisticated monitoring systems that provide online clearances, isothermal dialysis, high flux membranes and convective modalities such as haemofiltration and haemodiafiltration
More external articles on the history of dialysis:
- http://www.renalmed.co.uk/history-of/haemodialysis
- http://www.washington.edu/alumni/columns/march10/shunt.html
- https://www.davita.com/treatment-services/dialysis/the-history-of-dialysis
- http://historyofnephrology.blogspot.co.uk/2010/04/dialysis-for-endstage-renal-failure.html#!/2010/04/dialysis-for-endstage-renal-failure.html
The history of kidney transplantation
(This is an extract of a longer article which can be found here: http://www.renalmed.co.uk/history-of/renal-transplant )
Working in some obscurity in Kherson (Ukraine), Yuri Yurijevich Voronoy (1895-1961) performed six human kidney allografts between 1933 and 1949 - the kidneys being transplanted into the thigh. The first 'successful' one, in 1933, was the first human-to-human kidney transplant (Voronoy, 1936; Hamilton, 1984).The kidney was ABO-incompatible (B to O), and was rejected.
Sporadic further efforts at renal allotransplantation (genetically dissimilar donor and recipient) were made in the ensuing 15 years without effective immunosuppression. It wasn't until the second world war and work with skin grafts that Thomas Gibson and Peter Medawar showed that rejection of skin grafts was an immunological process. This work showed that the body's rejection of foreign tissue was indeed an immune response.
Medawar continued in this field and his historic achievements established the field of modern transplant immunology, and he shared the Nobel prize in medicine with Sir Frank Macfarlane Burnet in 1960.
The first successful transplant took place in Boston in 1945 on a patient with acute kidney injury. A deceased donor's kidney was temporarily connected to the patient via blood vessels and placed in a plastic bag. After 4 days the patient's kidney recovered its function and the deceased donor's kidney was removed.
Five years later, in 1950, the first success intra-abdoeminal cadaveric renal transplant occurred in a patient with CKD. It was carried out on 17th June, by Richard Lawler (1895-1982) at the Little Company of Mary Hospital, Chicago. He removed a kidney from a deceased donor, and placed it into his patient, Ruth Tucker (44 years), who had polycystic kidney disease (removing one of them at the same time) (Lawler, 1950).
 To everyone's surprise, the kidney worked for at least 53 days. At ten months, it was found to be shrunken, discoloured and rejected, and was removed. The patient lived for another five years.
To everyone's surprise, the kidney worked for at least 53 days. At ten months, it was found to be shrunken, discoloured and rejected, and was removed. The patient lived for another five years.
In a historic 12 day period in January 1951, René Küss and Charles Dubost (in Paris) and Marceau Servelle (Strasbourg) performed the first renal transplants in France. A total of nine patients were transplanted, all nine patients rejected their grafts. Rene Kuss' wrote in 1951, "about some cases of renal allograft in human .. in the present state of knowledge, the only rational basis for kidney replacement would be between monozygotic twins". By hypothesis the only known way of avoiding rejection.
In December 1952, the French physician, Jean Hamburger, working with the urologist Louis Michon at the Hospital Necker (Paris), reported transplanting a kidney from a live volunteer donor (Michon, 1953). The kidney, which was donated to a 16 year carpenter Marius Renard from his mother, functioned well and for 3 weeks before being rejected by the non-immunosuppressed recipient. Her son was probably in ATN following blood loss, and had a (congenital) single kidney. This was the first successful living kidney transplant, albeit lasting for a short period. Hamburger probably also coined the term 'nephrology'.
In 1954, Richard Herrick, a 24 year-old patient with chronic kidney disease and severe hypertension secondary to glomerulonephritis and an identical twin, Ronald, underwent a live donor transplant by surgeon, Joseph E Murray in Boston, USA. The kidney lasted for 8 years, when Richard Herrick died of a myocardial infarction, his glomerulonephritis having recurred.
Transplantation in the UK.
Soon after the success in Boston, progress started in the UK. The first deceased donor transplant (unsuccessful) was performed in the UK in 1955, at St Marys Hospital.
In July 1959 the first successful deceased donor renal transplant in the UK was performed by 'Fred' Peter Raper, a urologist, in Leeds. The team in Leeds used cyclophosphamide as an immunosuppression. The patient died, with a working transplant eight months later, of a viral infection.
On 30th October, 1960, the first successful living kidney transplant in UK was performed on identical twins. Sir Michael Woodruff (1911-2001) operated on the patient, a 49 year old man; and Mr James A Ross, on the donor (Woodruff, 1961). Following these successful operations, the donor resumed work 3 weeks after the operation; the patient returned to work after 15 weeks. The patient lived for a further 6 years before dying from an unrelated disease.
In November 1960 the first successful non-twin sibling living transplant in the UK was carried out by Hopewell. This was also the first use of 6-MCP in humans, and the first use of prednisolone in the UK. 'Success' was difficult to define in these early transplants. This patient died after seven weeks.
Immunosuppression
In 1962, the first successful kidney transplanted, using the new immunosuppressive drug azathioprine, from a deceased donor occurred in Boston USA; the kidney functioned for 21 months.
In 1972 Jean Borel discovered the immunosuppressant properties of cyclosporine, a drug widely used in organ transplants between unrelated people to reduce the activity of the patient’s immune system and so the risk of rejection. Cyclosporine was approved by the FDA for use as an immunosuppresant drug in 1983. It was recognized as the most successful anti-rejection medication developed to date.

Indefinite functioning of transplanted organs with little or no immunosuppression (with all its complications) remains the target for future generations. Hence non-surgical components of organ transplantation - immunosuppression, tissue matching, and organ procurement (and preservation) - have not yet delivered excellence in the 21st Century.
Transplantation today
Transplantation today has benefitted enormously from these early medical pioneers and their patients.
- Laparoscopic surgery to improve live donor transplatation
- Immunosuppression consists of a combination of 3 medicines, typically Tacrolimus, Mycophenolate Mofetil and Prednisolone.
- Antibiotic and antiviral medication help to stave off many of the known problems following a transplant
- Monitoring regime post-transplant - blood tests check for early signs of problems
- Related monitoring for skin cancer, bone density problems and cardiovascular issues.
- Needle biopsies help identify changes to the kidney graft that allow for earlier interventions while minimising patient risk.